Immune-Mediated Inflammatory Diseases
How the immune system works
The immune system provides a defense mechanism against foreign antigens, which includes infectious agents. 1 The immune system’s crucial role in protecting the body against pathogens depends on complex interactions between organs, tissues, cells, and molecules. 2
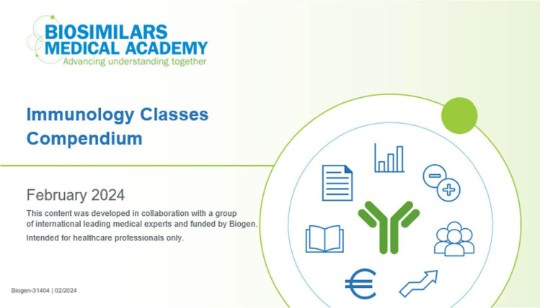
The immune system can be described as comprising three different lines of defense: 1) anatomical and physiological barriers; 2) innate immunity; and 3) adaptive immunity (Figure 1). Failure in any one of these components significantly increases susceptibility to infection from external agents. 1,3
Physical barriers are a first line of defense against infectious agents. In addition to this, when a host organism encounters a foreign antigen, two different but connected parts of the immune system are activated: the innate (non-specific) and adaptive (specific) immune response. Both have certain physiological factors that enable the host to recognize antigens and to neutralize, eliminate, or metabolize the harmful agent, with an increased complexity in their antigen-recognition mechanisms. Innate immunity represents the initial immune response, mounted within minutes of encountering an antigen, while adaptive immunity is the later stage of defense, which is antigen-dependent. Adaptive immunity can be separated in two mechanisms: humoral and cell-mediated immune responses. 1-3
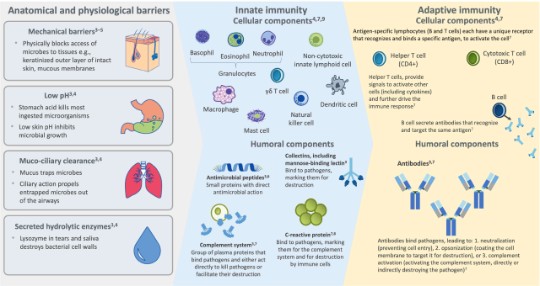
Figure 1. Different lines of defense of the immune system. Adapted from references 3-9.
Innate immunity, found in all animals and plants, represents the first line of defense in the immune response. It offers immediate protection against invading antigens in contact with the human body. This defense mechanism is characterized by being antigen-independent and providing a rapid response, but with no ability to memorize a pathogen to allow for future responses. Components of the innate immune response recognize conserved molecular patterns that are expressed on different pathogens. 1,3,10
Adaptive immunity (or the acquired immune response) is found only in higher vertebrate lifeforms, and forms the second line of defense, which is antigen-dependent, and antigen-specific. It is activated by the innate immune system. The adaptive immune system components have slower temporal dynamics and greater specificity in their responses, compared with the innate response. Adaptive immunity is activated upon antigen contact and is characterized by an enormous set of effector molecules and cells that are able to efficiently recognize and potentially eliminate pathogens. Adaptive immunity also establishes immunological memory, which provides the capacity to protect the body from re-infection by the same pathogen in future. 1,3,10
Difference between innate and adaptive immune systems 1,3,10
Watch this interactive e-learning module and learn more about the principles of clinical immunology, the immune system and its players, including an overview about innate and adaptive immunity, and the following topics:
- Defense mechanisms of the body
- Anatomical and physiological barriers
- Signaling pathways
In this interactive e-learning module you will discover more about the immunological disease continuum and the mechanisms of IMIDs, including the following topics:
- Immunopathogenesis
- Activation of helper T cell responses
- Activation of B cell responses by T cells
- Potential roles of B cells in the pathogenesis of RA
Find the full curriculum from the previous interactive e-learning module in the Immunology Classes Compendium, developed in collaboration with a group of internationally leading medical experts, which explores the following topics:
What are immune-mediated inflammatory diseases (IMIDs)?
Immune-mediated inflammatory diseases (IMIDs) are a group of seemingly unrelated conditions that share common inflammatory pathways, which drive inappropriate or excessive immune response (Figure 2). In IMIDs, such as rheumatoid arthritis (RA), inflammatory bowel disease (IBD) and psoriasis (PsO), the immune dysregulation may affect any organ system, resulting in significant morbidity, reduced quality of life (QoL) and premature death. Although the exact cause of IMIDs is unknown, it has been established that an imbalance, or dysregulation, in inflammatory cytokines is crucial to their pathogenesis. 11,12
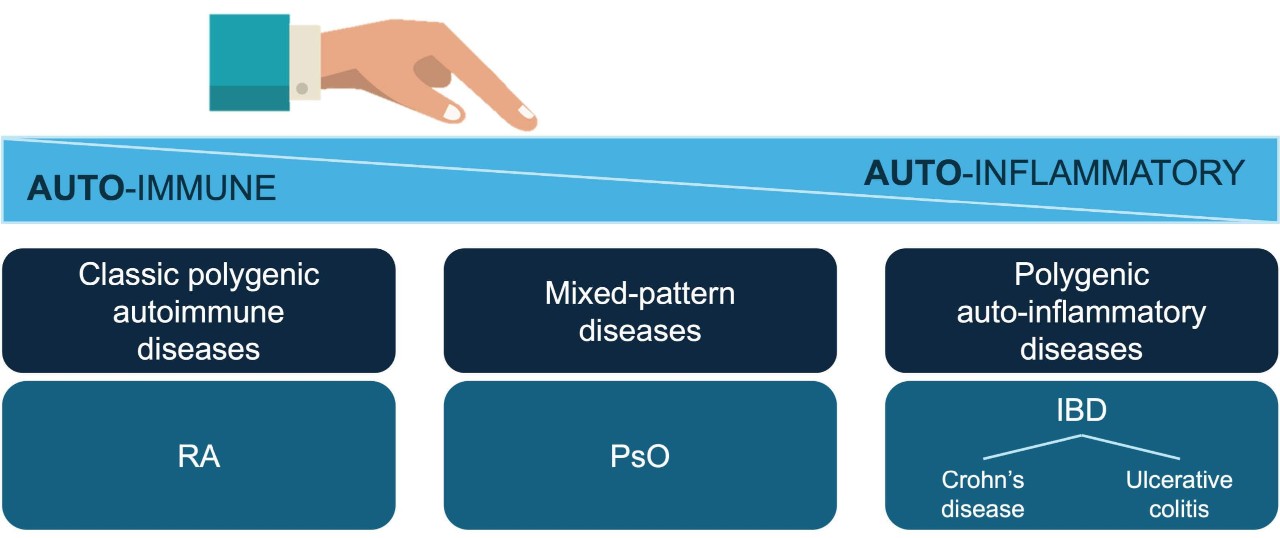
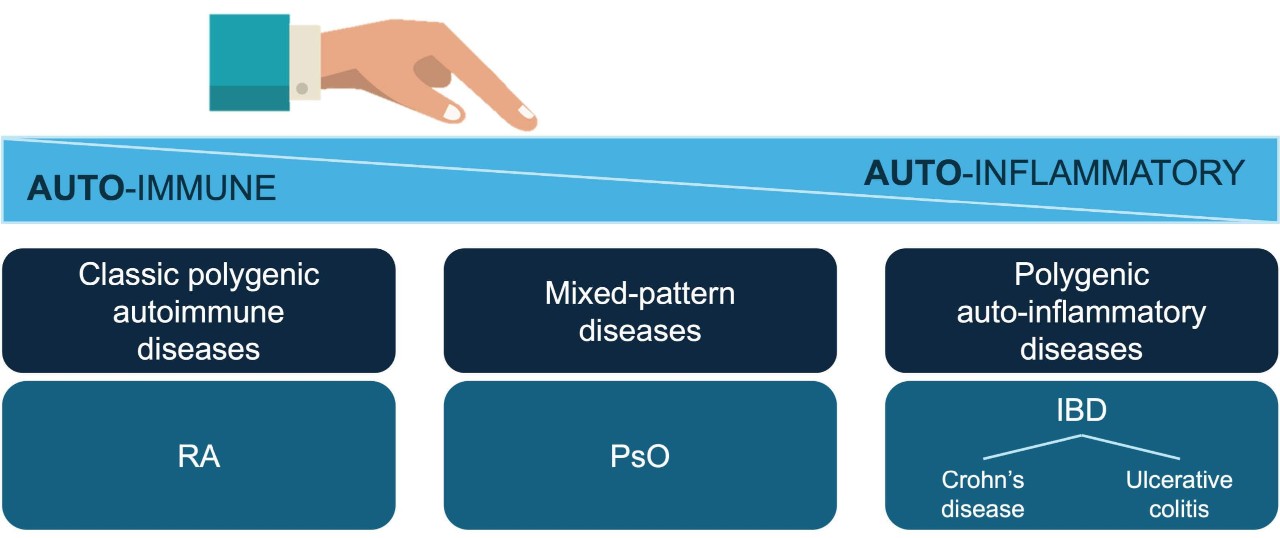
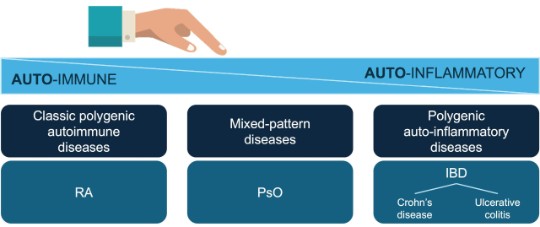
Figure 2. Overview of IMIDs
The pathophysiology, disease burden and treatment of IMIDs
IMID prevalence is estimated at 5–7% in Western societies. Genetic predisposition is a key determining factor in IMID susceptibility; animal model research has identified several genes that contribute to autoimmunity. It is also known that several IMIDs share similar environmental triggers, such as infection and trauma. Multiple IMIDs can occur within the same patient, and several IMIDs can co-exist within the same family (Figure 3). 11,12
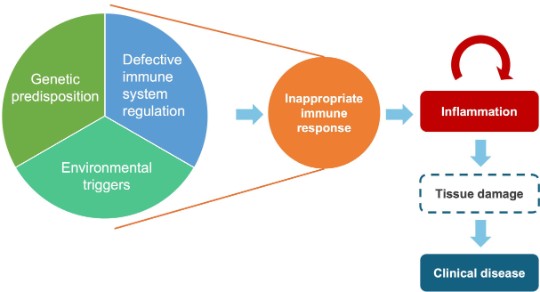
Figure 3. Mechanisms of IMIDs. Adapted from references 13,14.
IMIDs are progressive, chronic diseases that require timely intervention and continuous management. Targeted biologic therapies have revolutionized IMID therapy, 11 particularly taking into consideration that all the different pathologies present similar therapeutic goals. IMID treatment aims for rapid control of inflammation, prevention of tissue damage, improvements to QoL and, if possible, achieving long-term disease remission. Treatment should be initiated early, to achieve optimal clinical outcomes in patients. 11,15
Current treatment guidelines reserve biologics for patients with more severe disease and/or for patients who have failed to respond to other treatments with different mechanisms of action. Access to biologic therapies can be further limited by the implementation of local eligibility and reimbursement criteria, creating unmet medical needs in many countries worldwide. 15
Learn through these video animations key scientific insights about the pathophysiology of IMIDs, and the pathophysiology, disease burden, and treatment of RA.
1.Marshall JS, et al. Allergy Asthma Clin Immunol. 2018:14(Suppl 2):49.
2.Vaillant AAJ, Sabir S, Jan A. Physiology, Immune Response. Treasure Island (FL): StatPearls Publishing; 2025.
3.Turvey SE, Broide DH. J Allergy Clin Immunol. 2010;125(2 Suppl 2):S24–S32.
4.Warrington R, et al. Allergy, Asthma & Clinical Immunology. 2011;7(Suppl 1):S1.
5.Delves PJ, Roitt IM. N Engl J Med. 2000;343(1):37–49.
6.Oppenheim JJ, et al. Ann Rheum Dis. 2003;62(Suppl 2):ii17–ii21.
7.Murphy K, Weaver C. Janeway’s Immunobiology (9th ed). New York: Garland Science, 2017.
8.Salazar J, et al. Cardiol Res Pract. 2014:2014:605810.
9.Artis D, Spits H. Nature. 2015;517(7534):293–301.
10.Tomar N, De RK. Methods Mol Biol. 2014;1184:3–12.
11.Kuek A, Hazleman BL, Ostor AJK. Postgrad Med J. 2007;83:251–260.
12.Williams JP, Meyers JA. Am J Manag Care. 2002; 21(Suppl):S664–S681.
13.Ermann J, Fathman CG. Nat Immunol. 2001;2(9):759–761.
14.Rosenblum MD, Remedios KA, Abbas AK. J Clin Invest. 2015;125(6):2228–2233.
15.Edwards CJ, et al. Expert Opin Biol Ther. 2019;19(10):1001–1014.
Abbreviations:
Steering committee
Chairs:
Prof. Hubertus H. Nietsch
Director of the Medical Clinic 1 St. Elisabeth and St. Barbara Hospital Halle (Saale), Germany
Prof. Nietsch, MD serves as Director of the Medical Clinic 1 St. Elisabeth and St. Barbara Hospital Halle (Saale), Germany. He also holds a faculty position at Albany Medical Center, NY, USA. He completed his medical training at Munich University and University College Dublin, Ireland, followed by postgraduate fellowships at the University of Vermont and University of Washington, Seattle.
His main interests in gastroenterology are the management of patients with complex GI problems, including inflammatory bowel disease and interventional endoscopy. He is a member of DGVS, ASGE and AGA. He serves on the editorial board of national and international GI journals.
Prof. Nietsch has no disclosures to share
Prof. Luis Puig
Director of the Department of Dermatology, Hospital de la Santa Creu i Sant Pau (HSCSP), Barcelona, Spain
Prof. Luis Puig Sanz is Director of the Department of Dermatology, Hospital de la Santa Creu i Sant Pau (HSCSP), and Professor of Dermatology at the Universitat Autònoma de Barcelona (UAB) Medical School, both in Barcelona, Spain.
To date, Prof. Puig’s clinical research has focused on psoriasis, atopic dermatitis, urticaria, and hidradenitis suppurativa, and he has participated in over 100 clinical trials and research projects. He is considered to be a key opinion leader in this field, both nationally and internationally, having conducted 600 presentations at national and international conferences, workshops, and seminars. He is co-author of the Dermatology Textbook "Dermatología Clínica", edited by Prof. Carlos Ferrándiz, widely accepted and recommended in many Medical Schools of Spain and Latin America. He is a member of the Editorial Board of many dermatology journals including Dermatology, Actas Dermosifiliográficas, Journal of Psoriasis and Psoriatic Arthritis, Medicina Cutánea Latinoamericana, Piel, Medicina Clínica, and reviewer for Archives of Dermatology, British Journal of Dermatology, Dermatology, Journal of Investigative Dermatology, Acta Dermato-Venereologica, and the Journal of the European Academy of Dermatology, among others.
Prof. Puig Sanz is Co-chair of the Task Force on Psoriasis for the EADV, was a member of the EADV Board of Directors and a member of the EADV Nomination and Elections Committee (2013−19). He is currently Councillor (2012−) and a board member (2018−) of the International Psoriasis Council, and a member of the Skin Inflammation and Psoriasis International Network and the Fondation René Touraine, of which he was President until 2019. He is a member of several other scientific committees including the European Scientific Committee - Dermatology, European Center for Clinical Excellence, and European Dermatology Forum.
Disclosures:
Luis Puig Sanz receives honoraria for speaking and consulting from: AbbVie, Almirall, Amgen, Baxalta, Biogen, Boehringer Ingelheim, Celgene, Fresenius-Kabi, Janssen, JS BIOCAD, Leo-Pharma, Lilly, Mylan, Novartis, Pfizer, Regeneron, Roche, Sandoz, Samsung-Bioepis, Sanofi, UCB.
Prof. Puig Sanz has participated in company-sponsored speaker’s bureaus for: Celgene, Janssen, Lilly, Novartis, Pfizer.
Grants and research support have been received from: AbbVie, Almirall, Amgen, Boehringer Ingelheim, Celgene, Janssen, Leo-Pharma, Lilly, Novartis, Pfizer, Regeneron, Roche, Sanofi, UCB.
Prof. Hendrik Schulze‑Koops
Head of the Department of Rheumatology, Munich University Hospital, Munich, Germany
Prof. Hendrik Schulze-Koops received his doctorate of medicine from the University of Hamburg, Germany, in 1988 for his work on the arthritogenic factors of Yersinia. He was promoted to Professor of Clinical Immunology at the University of Erlangen-Nuremberg, Germany, in 2006, and since then has held the position of Professor of Internal Medicine and Rheumatology at Munich University Hospital, Germany. With nearly 30 years' experience in the field of clinical immunology, Prof. Schulze-Koops is one of the foremost authorities in rheumatism.
Prof. Schulze-Koops' current research focuses on cellular and molecular pathogenesis of autoimmune diseases, and he is currently leading research into mechanisms of sustained autoimmune T-cell activity in diseases, such as rheumatoid arthritis with the two important aspects of increased activity of inflammatory effector T cells and decreased functionality of regulatory T cells.
Disclosures:
The Division of Rheumatology and Clinical Immunology of the University of Munich receives financial support from AbbVie, Amgen, AstraZeneca, Biogen, BMS, Celgene, Celltrion, Fresenius, Gilead, GSK, Hospira, Janssen-Cilag, Lilly, Medac, MSD, Mundipharma, Mylan, Novartis, Pfizer, Sanofi-Aventis, Hexal Sandoz, Shire Baxalta, Sobi, Roche, UCB
Hendrik Schulze-Koops receives honoraria for lectures and consultations from AbbVie, Amgen, AstraZeneca, Biogen International, BMS, Boehringer Ingelheim, Celgene, Celltrion, Gilead, GSK, Hospira, Janssen-Cilag, Lilly, Medac, MSD, Merck, Mundipharma, Mylan, Novartis, Pfizer, Sanofi-Aventis, Hexal Sandoz, Roche, UCB
Steering Committee members
Dermatology
Prof. Giampiero Girolomoni
University of Verona, Italy
Prof. Miriam Wittmann
University of Leeds, UK
Prof. Peter Weisenseel
Dermatologikum Hamburg, Germany
Gastroenterology
Prof. Yoram Bouhnik
Hôpital Beaujon, Paris Diderot University, France
Prof. Flavio Caprioli
Università degli Studi di Milano, Italy
Prof. João Gonçalves
University of Lisbon, Portugal
Dr Fraser Cummings
Southampton General Hospital, UK
Rheumatology
Prof. Maria Cuadrado
Clínica Universidad de Navarra, Madrid, Spain
Prof. Bruno Fautrel
Université Pierre et Marie Curie, Paris, France
Prof. Tore Kvien
University of Oslo, Norway
Prof. Maurizio Cutolo
University of Genova, Italy
Prof. Carlo Selmi
Rheumatology and Clinical Immunology, Humanitas Research Hospital, Humanitas University Milan, Italy
Dr Raj Sengupta
Royal United Hospitals and University of Bath, UK
Prof. Alla Skapenko
Ludwig-Maximilians-Universität Munich, Germany
Prof. Peter Taylor
University of Oxford, UK